Safest Height for Wall-Mounted Sharps Containers
What is the ideal height for a wall mounted sharps container?
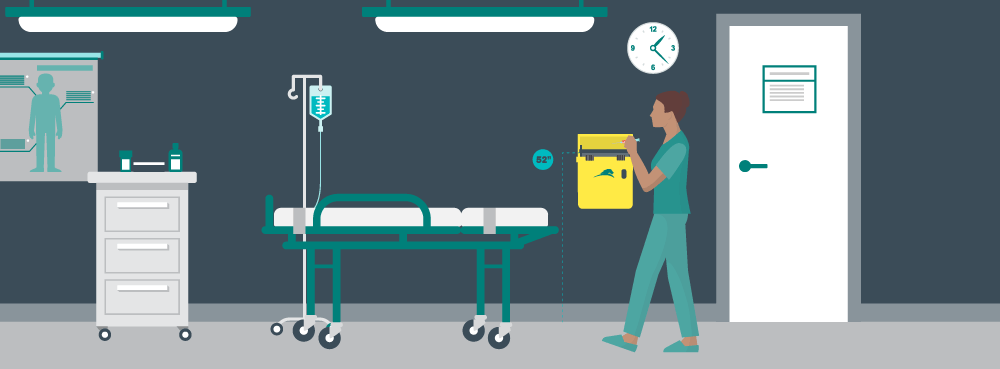
Great question! We’re glad you asked. According to NIOSH, an ideal standing installation height for a fixed sharps container is 52” – 56” from the floor. At Daniels, we follow the NIOSH guidelines for the mounting height of our sharps containers with each container mounted 52” from the floor. Our decision to choose the lower height within the NIOSH scale is based on the following considerations:
- The 1998 NIOSH Guideline on sharps container height utilizes 1979 female height data and doesn’t take into account the diversity of recruitment from shorter-stature countries that exists today
- High-mounted sharps containers are associated with sharps injuries, low mounted sharps containers are not3-6
- Earlier guidelines were based on top-loading sharps containers, they did not take into account the “letterbox design” of a Sharpsmart container with its retractable safety tray
- To ensure healthcare worker and child safety, a healthcare worker should be able to see inside the aperture of the container to ensure there are no misplaced sharps
It is common to wall-mount containers in patient rooms so that they are “as close as feasible to the point of generation of the sharp.2 In 2001, Point of Use container-placement became law in Canada and the regulations and guidelines state:

CDC NIOSH Sharps Container Guidelines,
“…containers should be placed within arm’s reach and below eye level at their point of use.”
Positioning sharps containers at point-of-care in patient rooms
A sharps container study conducted in 2012 and published in the Journal of Infection Prevention1 compared use of sharps containers mounted in a fixed position in patient rooms versus sharps containers located outside of the patient environment. The six year study saw container-associated sharps injuries reduce by 49%, citing the location of the container as one of the leading indicators for the significant decrease. The study can be read here. Conclusions were drawn that sharps should not be hand-transported to a distant container, and while carrying sharps containers directly to the bedside eliminates “transport risk,” use of smaller disposable sharps containers may increase risk of container associated needlestick injuries.
In our 32 years servicing the global healthcare industry and being proactive advocates for safer sharps container standards, we have seen firsthand that adopting sharps containers that are functional, accessible, secure from patient or visitor tampering, visible and convenient to use will decrease the risk of percutaneous sharps injuries. Sharps containers should be installed to provide one-step, one-hand deposition of a sharp and should be of a size equivalent to the volume of sharps being generated.
Sharps container usage should ideally be part of an institutional process that:
- Promotes worker education and training in the proper use of sharps disposal containers and safety devices
- Reduces risk of disposal related injuries
- Promotes compliance with standard precautions
- Supports surveillance of sharps injuries
- Eliminates avoidable risk in the handling, disposal and transportation of sharps.
References
1. Grimmond T and Naisoro W. Sharps injury reduction: A 6-year, 3-phase study comparing use of a small patient-room sharps disposal container with a larger engineered container., J Infect Prev 2014;15 (5):170-174.
2. U.S. Department of Labor, Occup. Safety & Health Admin. Standard 29 CFR: Bloodborne Pathogens – 1910.1030.
3. Weltman AC, Short LJ, Mendelson MH, Lilienfeld DE and Rodriguez M. Disposal-Related Sharps Injuries at a New York City Teaching Hospital. Infect Control Hosp Epidemiol 1995; 16:268
4. (Anonymous) In-room sharps disposal systems reducing needlesticks. Hospital Infection Control. 1988;15(7):85–89.
5. (Anonymous) The needlestick that changed her life. Hospital Infection Control & Prevention 2010;Nov 1. https://www.ahcmedia.com/articles/20911-the-needlestick-that-changed-her-life
6. Tereskerz PM, Bentley M, Coyner BJ, Jagger J. Percutaneous Injuries in pediatric health care workers. Adv Exp Prev 1996;2(5):1-3.
Let's Talk!
Your time is valuable, and we don’t want to play hard to get. You can either phone us directly on the details listed on our contact page, or feel free to fill out this short form and one of our team members will get back to you as quickly as possible.
